Ectopic Atrial Rhythm (EAR) is a term used to define the atrial site that drives the heart rhythm during rest in lieu of a classic sinus node P-wave. It is a term of broad applicability and is meant to indicate that the normal sinus P-wave is not present, at least for the time that EAR is present on the ECG. For the Carnation Ambulatory Monitor, sinus P-waves will have the same appearance commonly seen on the 12-lead ECG aVF lead of an upright, smoothly curved P-wave similar to the upright half of a sine wave.
At Bardy Diagnostics, we use the term EAR to indicate an atypical P-wave morphology that drives the resting rhythm.
It often indicates that the atrial pacemaker is located somewhere else in the atria. Alternatively, it could indicate that the spread of atrial activation from the sinus node is atypical resulting in a P-wave morphology that is not classic. Realistically and practically, we cannot discern the difference between these two but use the same terminology to draw the physician’s attention to this finding as it might influence patient management. Causes of true EAR or apparent EAR can be due to normal or abnormal variations in autonomic function, drug effect, anatomic abnormalities, or, no abnormality whatsoever. Its occurrence remains a mystery in most instances. Regardless of the cause, it may or may not be an abnormal finding (often it is not) and is a diagnosis provided by BDx to allow the managing physician a more nuanced understanding of their patient’s cardiac rhythm.
Like Atrial Tachycardia (AT), Ectopic Atrial Tachycardia (EAT) has a narrow QRS complex as is manifested with sinus rhythm but with an abnormal P-wave driving heart rates > 100bpm. Unlike AT, EAT has a sense of enhanced automaticity above that of the sinus node and arising somewhere else in the atria. It is rarely very rapid, with rates being relatively modest, often competing with sinus tachycardia. While the location of the ectopic focus can be in either atrium, right atrial EAT appears somewhat more common than the left given P-wave morphology considerations.
EAT is significantly less common than AT, that tends to arise abruptly without warmup.
The clinical significance of EAT is not clear and is similar to that seen with EAR albeit very slightly more likely to represent some form of cardiac rhythm dysfunction by virtue of its higher rate.
59-year-old female with no known underlying heart disease other than a history of palpitations, complaining of dizziness and lightheadedness. This patient had frequent transitions of normal sinus rhythm to an ectopic atrial rhythm as well as lest frequent occasions of ectopic atrial tachycardia competing with some sinus tachycardia at rates up to 141 bpm. See ECG strips below.
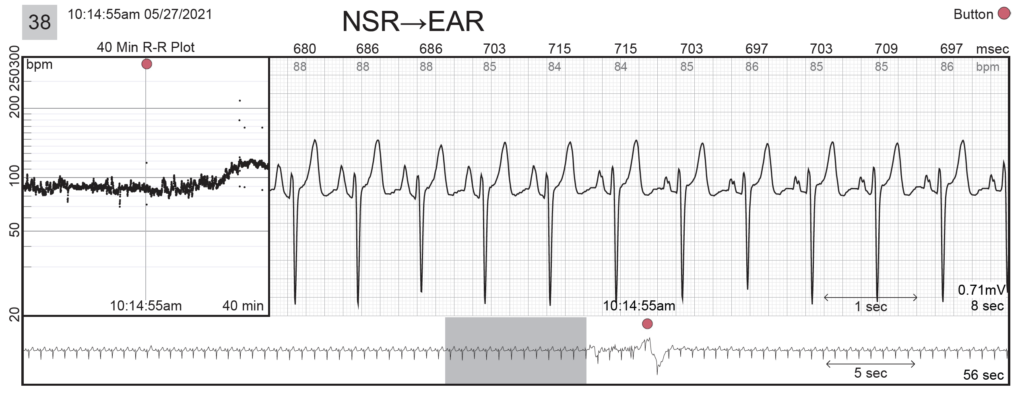
Example Strip #38: Normal sinus rhythm with transitional ectopic atrial rhythm with a notch p-wave, in which the patient pressed the button on the monitor (red dot).
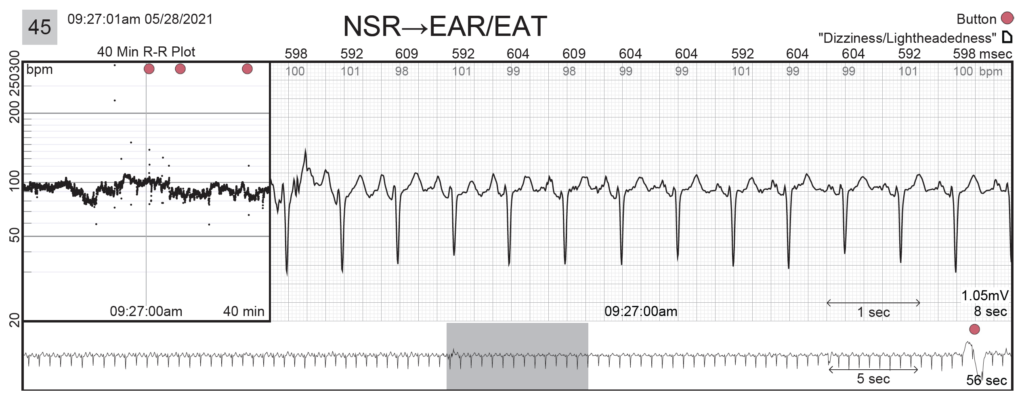
Example Strip #45: The tracings above and below show normal sinus rhythm with transitional ectopic atrial rhythm (EAR)/ectopic atrial tachycardia (EAT) with heart rates up to 104 bpm with a notched p-wave. On this occasion, as well as others over the course of the recording, the patient pressed the symptom button on the monitor (red dot) and complained of “Dizziness/Lightheadedness” (white paper icon). This is a finding suggesting the patient’s extreme sensitivity to minor changes in cardiac activation.
US-FLC199-230029 v1.0